Patient Education
- Home
- Patient Resources
- Current: Patient Educations
What Is Age-Related Macular Degeneration?
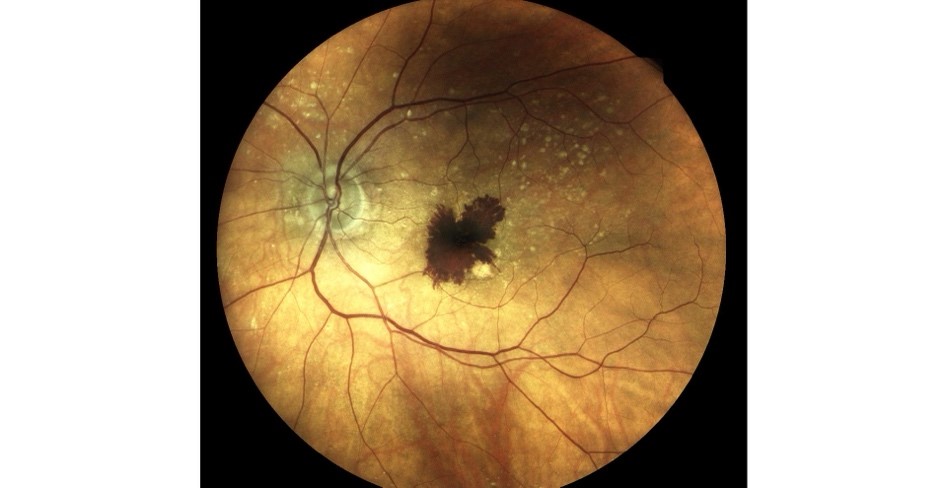
Age-related macular degeneration (AMD) is a leading cause of irreversible vision loss worldwide and the primary cause of blindness in individuals aged 55 years and older. It accounts for 6-9% of legal blindness globally and is projected to affect 288 million people by 2040. It is a common eye condition that primarily affects the macula—the small, central portion of the retina responsible for sharp, detailed vision. This central vision is essential for everyday activities like reading, driving, and recognizing faces.
What causes AMD?
AMD is multifactorial, stemming from a combination of aging, genetics, and environmental influences. As we age, natural wear and tear on the retinal tissues occurs, and genetic factors can predispose some individuals to the condition. Additionally, lifestyle factors such as smoking, poor diet, and excessive sun exposure may contribute to oxidative stress and inflammation, which accelerate the deterioration of the macula. These factors collectively lead to the buildup of cellular debris and drusen—small yellow deposits beneath the retina—that are often the first sign of AMD.
Classification
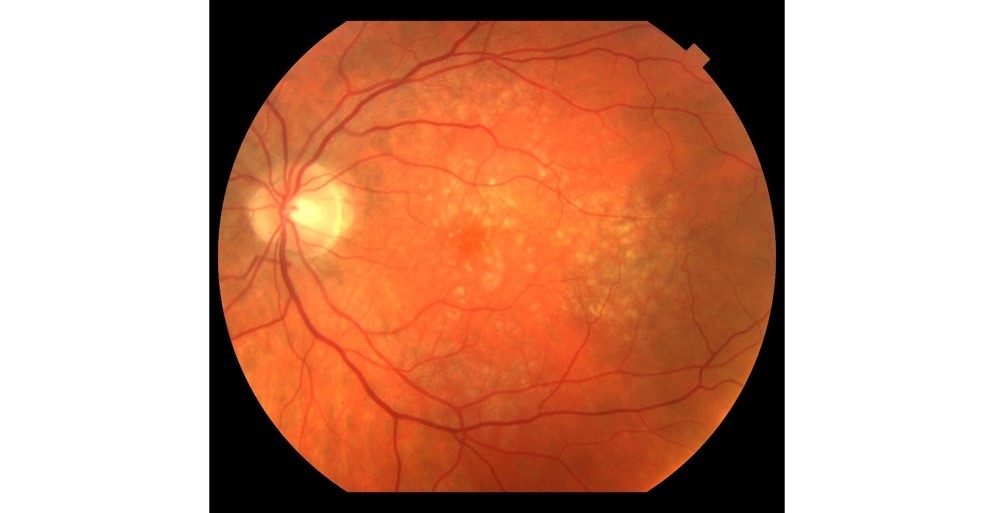
AMD is broadly classified into two main categories—dry (atrophic) and wet (neovascular)—each with distinct characteristics and progression patterns.
Dry AMD
Dry AMD, which accounts for about 85-90% of all AMD cases, is further subdivided based on its severity and clinical findings:
- Early Dry AMD: At this stage, small drusen (yellow deposits) begin to appear beneath the retina along with subtle changes in retinal pigment. Many patients do not notice any vision loss during this phase, which is often detected during routine eye examinations.
- Intermediate Dry AMD: With progression, drusen become larger and more numerous, and pigment changes become more pronounced. This stage might begin to affect central vision, causing mild blurring or distortions.
- Advanced Dry AMD (Geographic Atrophy): In this advanced stage, there is a significant loss of retinal pigment epithelium and photoreceptors, leading to well-defined areas of atrophy in the macula. This irreversible damage can result in substantial central vision loss over time.
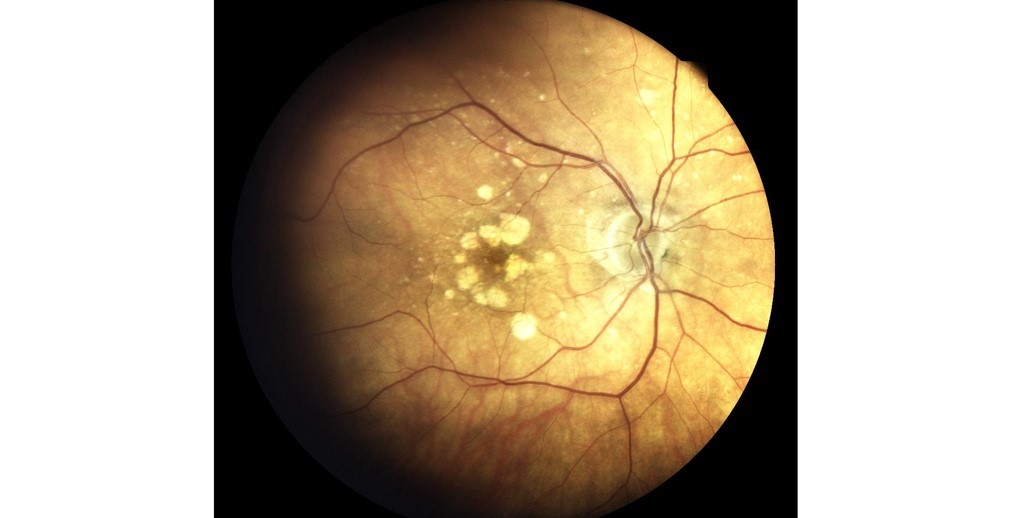
Wet AMD
Wet AMD, a more aggressive type, is characterized by the growth of abnormal blood vessels underneath the retina. These vessels may leak fluid or blood, leading to rapid damage of the macula and sudden vision loss. Wet AMD is typically classified based on the pattern of neovascularization (e.g., classic, occult, or minimally classic), which guides treatment decisions.
Symptoms
Patients with AMD often experience a slow, progressive loss of central vision. Early stages might include subtle blurring or distortions—images may appear wavy or crooked, a phenomenon known as metamorphopsia. As the disease advances, everyday tasks such as reading or recognizing faces become increasingly difficult. Notably, peripheral vision is usually preserved, which means that while central details fade, the overall field of vision remains largely intact.
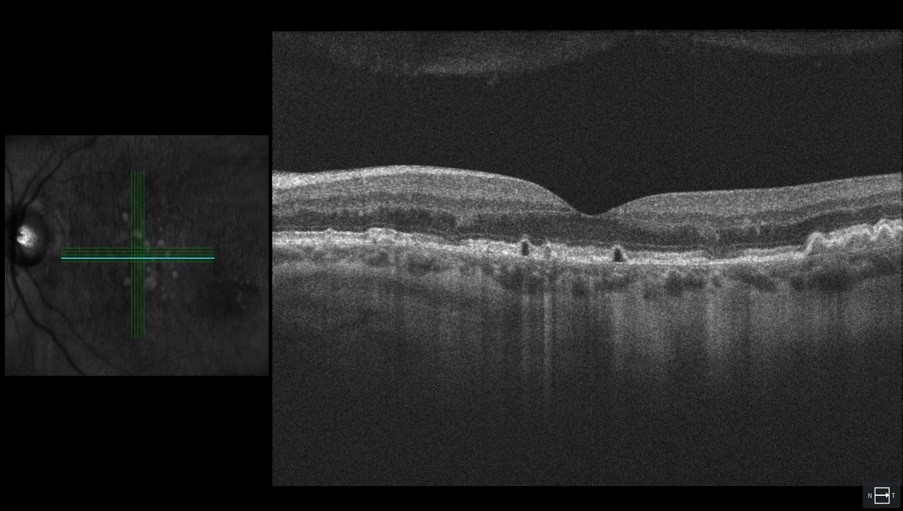
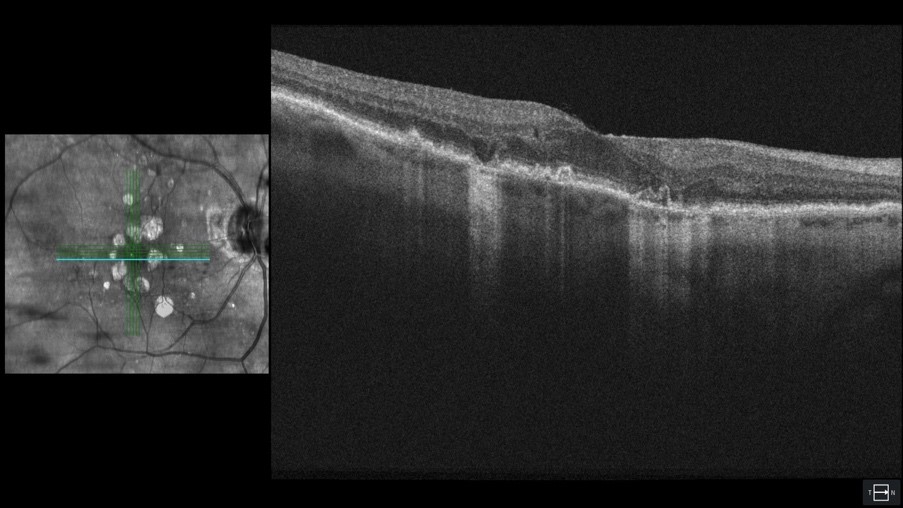
Diagnosis
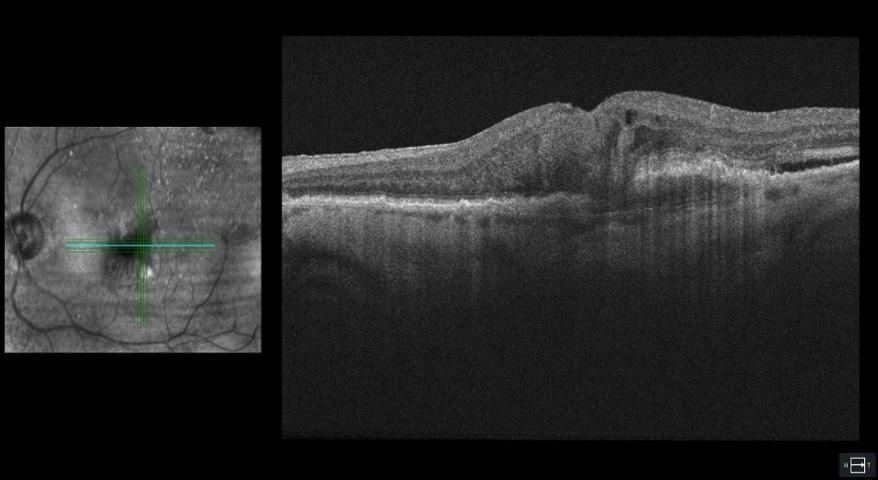
Early detection is the key to managing AMD effectively. A comprehensive eye examination, including visual acuity tests and the use of an Amsler grid, helps to detect distortions and subtle changes in vision. Non-invasive advanced imaging techniques such as optical coherence tomography, fundus autofluorescence and optical coherence tomography angiography are then used to capture detailed cross-sectional images of the retina. Invasive tests such as fluorescein angiography and indocyanine green angiography may be required in cases of neovascular AMD. These diagnostic tools enable us to assess the type and stage of AMD, allowing for a personalized treatment plan tailored to each patient's needs.
Treatment
Treatment for AMD is tailored to the type and severity of the condition, with distinct approaches for dry and wet forms. Advances in recent years have introduced new therapies that complement established treatments, offering hope for better outcomes and quality of life.
Dry AMD Treatment
For dry AMD, management typically involves lifestyle changes, such as quitting smoking and adopting a diet rich in antioxidants and AREDS2-based supplement regimen, which includes vitamins C and E, zinc, copper, lutein, and zeaxanthin to help maintain retinal health. For its advanced stage known as geographic atrophy two newer therapies have emerged:
Syfovre (pegcetacoplan)
This innovative treatment works by inhibiting a component of the complement system (complement factor C3), which plays a role in the inflammatory process that contributes to retinal cell damage. By slowing the progression of atrophy, Syfovre offers patients a promising option to preserve central vision for longer.
Avacincaptad Pegol
Another recently developed agent, avacincaptad pegol, targets the complement cascade in a slightly different way. Early studies have shown that it can reduce the rate of lesion growth in patients with geographic atrophy, offering an additional strategy in the fight against vision loss in dry AMD.
Wet AMD Treatment
Wet AMD is primarily managed with therapies that target abnormal blood vessel growth. These treatments are designed to inhibit vascular endothelial growth factor (VEGF), which is responsible for the formation and leakage of these problematic vessels. Key agents include:
Ranibizumab (Lucentis) and Aflibercept (Eylea)
These well-established anti-VEGF drugs have been the cornerstone of wet AMD treatment for years. Administered via intravitreal injections, they work to reduce fluid leakage and prevent further damage to the macula.
Bevacizumab (Avastin)
Although originally developed for cancer treatment, bevacizumab is widely used off-label for wet AMD. It is a cost-effective option that many clinicians consider for managing neovascularization.
Brolucizumab (Beovu)
A newer anti-VEGF agent, brolucizumab offers the potential for longer dosing intervals, which may reduce the treatment burden for patients while maintaining efficacy.
Faricimab (Vabysmo)
Representing the latest advancement, faricimab uniquely targets both VEGF-A and angiopoietin-2. This dual mechanism not only reduces abnormal vessel growth but also works to stabilize the blood vessels, offering a promising new option for patients with wet AMD.
In some cases, laser therapy or photodynamic therapy may also be considered. Each treatment is selected based on the individual's stage of AMD, overall eye health, and lifestyle considerations. Regular monitoring and follow-up are essential to adjust treatment strategies as the disease evolves.
About Us: Choroidal Analysis Research Lab
At the Choroidal Analysis Research Lab, we are revolutionizing eye care by harnessing cutting-edge artificial intelligence(AI) to interpret optical coherence tomography images, with a specialized focus on the choroid. Our research is dedicated to identifying robust, reproducible imaging biomarkers for AMD, addressing the current challenge where interpretations of these advanced scans can vary significantly among ophthalmologists.
By deploying advanced AI algorithms, we strive to standardize image analysis, enabling more accurate diagnoses, reliable tracking of disease progression, and precise evaluation of treatment responses. This innovative approach is not only critical for improving AMD management but also holds promise for enhancing the diagnostic accuracy for a range of other ocular conditions.
In partnership with NetraMind Innovations—a leader in integrating AI with medical imaging—we are committed to empowering eye care professionals with state-of-the-art tools that lead to improved patient outcomes and more consistent clinical decisions.
